For the first time in US history, the IRS will require taxpayers filing returns in 2018 to indicate if they had health coverage under the Affordable Care Act (ACA). The agency recently announced the change and indicated it won’t accept electronically filed tax returns that omit the information. Returns filed on paper may be suspended pending the IRS’ receipt of the health coverage information.
For The First Time Ever, IRS Requiring Taxpayers to Reveal Health Insurance Coverage
In its announcement about the change, the IRS stated that it had reviewed and discussed its process with National Taxpayer Advocate Nina Olson. “This process reflects the requirements of the ACA and the IRS’ obligation to administer the health care law,” the agency says in its announcement. Taxpayers should indicate if they and anyone else on their tax return had health coverage, qualified for an exemption from the coverage requirement or are making an individual shared responsibility payment.
For any month that taxpayers or members of their family didn’t have minimum essential coverage must claim or report a coverage exemption or make a shared responsibility payment on their returns, the IRS states. However, taxpayers may be exempt from the requirement for minimum essential coverage if they meet certain criteria nor will they have to make a shared responsibility payment. Instead, they’ll file Form 8965, Health Coverage Exemptions, with their federal return.
President Trump issued an executive order directing the government to limit burdens imposed by the ACA, pending repeal. In answer to that order, the IRS said it wouldn’t enforce the health care reporting information on 2016 returns filed in 2017. Taxpayers, though, still had to pay the shared-responsibility portion if they didn’t have coverage or qualify for an exemption.
According to legal experts the IRS is indicating that although the Trump administration may have leeway in how aggressively it enforces the mandate provision, it’s still in effect unless and until Congress specifically repeals it.
While many people thought they didn’t have to bother with reporting, and many insurers have raised rates anticipating that the lack of a mandate would lead to lower enrollments and higher costs for them, that’s not the case. Initially the IRS did not reject returns because the law was new.
The penalty is pretty steep; for those who don’t have coverage, it can range from $695 for an individual to a maximum of $2,085 for a family or 2.5 percent of AGI, whichever is higher. Not everyone without coverage would be penalized, though; if their income is too low or if the lowest-priced coverage costs more than 8.16 percent of their income, they’ll avoid the penalty.
That said, it’s not known how stringently the IRS will be in enforcing the mandate. But at least taxpayers will know whether they’re exempt from the penalty or whether they’re obligated to buy coverage.
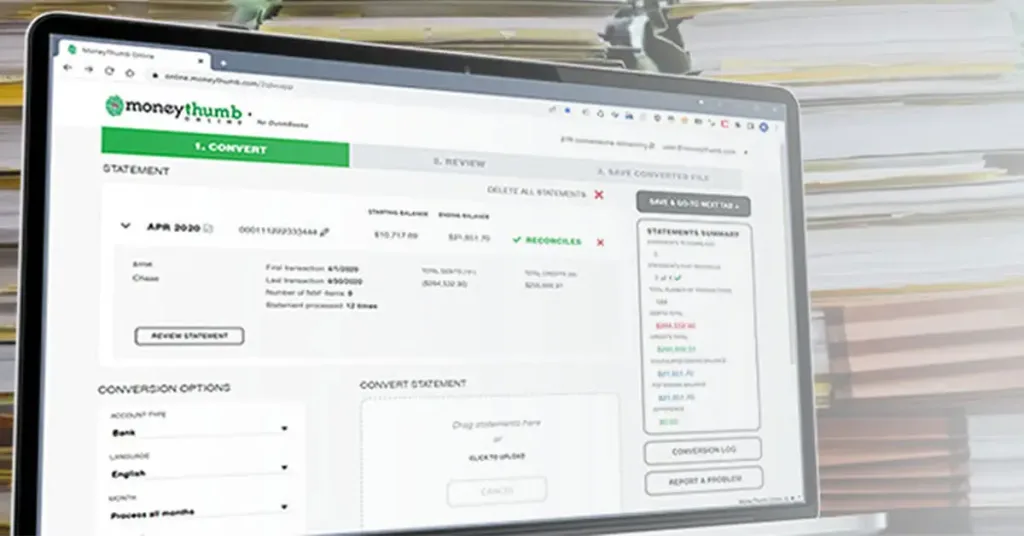
What kind of impact will this have on the accounting profession? It is a sticky situation, but looks like for the time being it is going to be unavoidable. What do you think?


















Add comment